Defining Substance Use Disorders: A Chronic Disease of the Brain
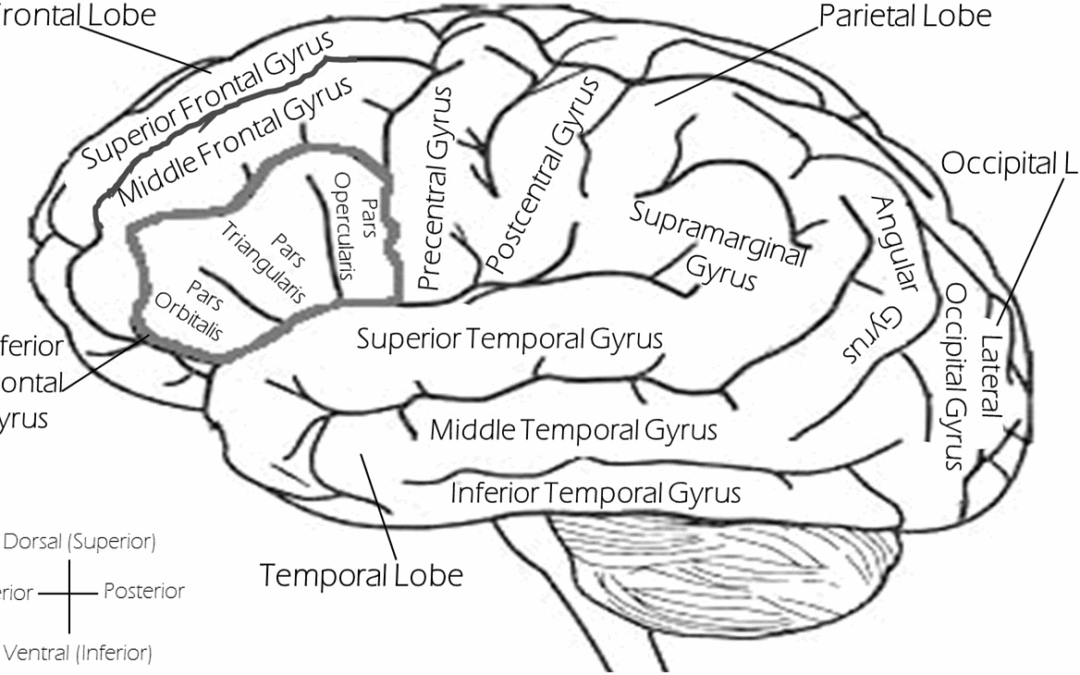
Substance Use Disorders are not mere lapses in self-control or moral failure—they are recognized as chronic, relapsing brain disorders characterized by compulsive drug-seeking and use, even in the presence of harmful consequences (1). The National Institute on Drug Abuse (NIDA) emphasizes this disease model, noting that repeated substance use leads to lasting changes in brain circuits, particularly those governing reward, stress response, and executive function (2).
Unlike acute intoxication, SUD involves long-term alterations in brain structure and function. These changes can affect learning, memory, impulse control, and emotional regulation. As a result, what begins as voluntary use can evolve into a powerful compulsion, often resistant to logic or willpower. Chronic drug exposure rewires the reward system, skewing it to prioritize drug-related stimuli while diminishing natural rewards (e.g., food, social interaction) (3).
Relapse is a hallmark of SUD. Approximately 40–60% of individuals relapse after treatment—a rate that mirrors other chronic diseases such as asthma and hypertension (4). This highlights that relapse is not a sign of failure but a characteristic of the disorder, underscoring the need for ongoing support and multifaceted interventions.
A fascinating yet under-discussed aspect is the role of epigenetics. Drug exposure can trigger epigenetic modifications (like DNA methylation and histone acetylation) that affect gene expression long after cessation. In animal models, even short-term exposure can create latent changes that heighten vulnerability to relapse (5). Additionally, some of these changes—even behavioral traits—can be passed to future generations, suggesting that addiction may influence descendants biologically.
This multifaceted understanding—from neurochemical rewiring to epigenetic inheritance—reveals why SUD is such a challenging, entrenched condition. It also provides hope: by targeting these mechanisms, we can develop more effective prevention and treatment strategies.
Scope and Scale: How Widespread Are Substance Use Disorders?
Substance Use Disorders affect millions worldwide. In the United States alone, 48.5 million individuals (16.7%) experienced an SUD in the past year, while 27.2 million (9.7%) had drug use disorders and 28.9 million (10.2%) had alcohol use disorders (6). These numbers reflect a pervasive public health crisis that extends across age, race, and socioeconomic status.
Youth exposure to drugs is particularly alarming. Studies show that substance use often begins in adolescence, significantly increasing the risk of lifetime SUD (7). Early exposure disrupts brain development and magnifies long-term vulnerability, underscoring the critical importance of early prevention and education programs.
Despite the high prevalence, only a fraction of individuals receive treatment. In 2023, just 14.6% of people with SUD and 18% of those with opioid use disorder received any form of treatment(8). This treatment gap is fueled by stigma, inadequate insurance coverage, and lack of access to evidence-based care. Alarmingly, 73% of those who recognize their problem eventually achieve recovery, highlighting both the potential for success and the need for intervention access (9).
The toll is significant: alcohol is the fifth-leading cause of preventable death in the U.S., responsible for approximately 88,000 yearly deaths (10). For other substances—opioids, stimulants, nicotine—the burden is also high, particularly in terms of overdose, chronic health issues, and economic costs estimated in the hundreds of billions per year.
These statistics paint a sobering yet actionable picture. SUDs are widespread but treatable, and scaling access to effective therapies could yield profound public health benefits.
3. Risk Factors: Why Do Some People Develop SUDs?
Substance Use Disorders emerge from the interaction of genetic, environmental, developmental, and psychological factors. Research estimates that 40–60% of addiction risk is attributable to genetics, particularly variations in dopamine pathway genes and neurotransmitter receptors (11). However, genetics is not destiny—environmental factors often tip the balance.
Early-life trauma and adverse childhood experiences (ACEs) are among the most potent predictors. Individuals who experienced four or more ACEs face a 11-fold higher risk of drug use and a 7-fold increase for alcoholism compared to those with none (12). Prolonged stress alters brain development, making reward and stress circuits more susceptible to substance seeking.
Epigenetic studies highlight that drug exposure itself can modify gene regulation, perpetuating vulnerability even after cessation. Remarkably, such alterations have been observed to transmit across generations in animal studies—a startling illustration of addiction’s long-term consequences.
Maintenance and relapse are strongly influenced by cue-reactivity: the exposure to drug-related stimuli (like paraphernalia or environments) that trigger intense craving and relapse. This highlights the importance of therapies targeting contextual and habitual triggers for effective long-term recovery.
While the concept of an “addictive personality” remains controversial, traits such as impulsivity, sensation-seeking, and emotional dysregulation do correlate with increased risk. These personality factors, combined with early trauma and genetics, create a powerful triad influencing vulnerability.
Treatment Approaches: What Works and Why Some People Relapse
Evidence-based treatments for SUDs include medications (like methadone, buprenorphine, naltrexone), behavioral therapies (CBT, Motivational Interviewing), peer support (12-step programs), and harm reduction (needle exchanges, naloxone access). Successful recovery often involves combinations of these approaches, tailored to the individual.
Medication-assisted treatment (MAT) for opioid use disorder is one of the most documented successes: Methadone and buprenorphine reduce overdose risk and mortality, yet in 2023 only 18% of those with opioid use disorder received MAT (13). Expanding access remains a priority.
Behavioral therapies like CBT and contingency management address cognitive distortions and reinforce sobriety with incentives. Additionally, novel interventions—virtual reality cue exposure and digital platforms—are being developed to reduce craving and support recovery outside clinics (14).
A cutting-edge development is the use of GLP-1 agonists like semaglutide (Ozempic) to reduce craving for alcohol and nicotine. Early trials show a 30% reduction in alcohol consumption and promising reductions in smoking, opening a potential new pharmacological frontier (15).
Even with these tools, relapse remains a challenge: about 40–60% relapse rates, similar to chronic diseases. But relapse signals a need for continued care—not failure—as outlined by the chronic disease model.
Intriguing and Lesser-Known Insights About SUDs
1. Epigenetic Transmission of Addiction Risk
Animal studies reveal that drug-induced epigenetic modifications in reward-circuit genes can be passed onto offspring, influencing vulnerability in the next generation.
2. Stigma as a Barrier to Treatment
Only ~7% of people with SUD receive any treatment. Digital research finds that stigmatizing language online deters help-seeking, but empathetic communication can foster engagement (16).
3. Alcohol as a Gateway Drug
Contrary to the cannabis gateway theory, research suggests alcohol may increase susceptibility to harder drugs by disrupting decision-making circuits in the brain (17).
4. Personalized Treatment Through Genetics
Pharmacogenomic studies are beginning to tailor addiction treatments. For instance, variations in dopamine D₂ receptor genes may predict response to medications and behavioral strategies (18).
5. VR-Cue Exposure Breakthroughs
Cutting-edge studies in the UK are deploying virtual reality simulations to help users manage triggers in a controlled environment—particularly for alcohol and cocaine craving.
The Path Ahead in the Fight Against Substance Use Disorders
Substance Use Disorders are complex but treatable conditions rooted in brain dysfunction, genetic predisposition, and environmental factors. With increasing research and evolving therapies—from GLP-1 drugs to VR-based interventions—we have new tools to reduce harm, support recovery, and prevent relapse.
What’s critical now is bridging the treatment gap, combating stigma, and integrating innovations into accessible care. If there’s one overarching truth, it’s this: SUD is a chronic illness, not a moral failure—and recovery is possible with the right support.

Recent Comments